Abstract
Background: Daratumumab is one of the most effective new myeloma drugs recently approved for relapsed/refractory multiple myeloma (MM), first in monotherapy in heavily pretreated patients, later in triplet combinations from first relapse, based on the results of the SIRIUS, POLLUX and CASTOR trials that showed good tolerability and high effectivity of daratumumab both in monotherapy and combined with lenalidomide or bortezomib. However, clinical trials are different from real world use for many reasons including less rigorous patient selection, greater flexibility with dosing and country specific funding restrictions making real world data very important for clinicians. Real world data regarding daratumumab use is currently very limited. In the Hungarian system, funding of daratumumab was initiated in December 2016, and required individual preapproved funding requests. Initially only monotherapy was reimbursed in double-refractory patients, but from 2018 triplet combination in earlier lines could start as well.
Aims and Methods: The aim of this study was to evaluate the efficacy and safety of daratumumab in the real world practice. We approached all centers in Hungary where daratumumab was used, in a retrospective analysis. The scope of this study was to analyze response rate, progression free survival (PFS), treatment duration, and adverse events (AEs). Statistical analyses were performed using the SPSS (version 20.0) software package.
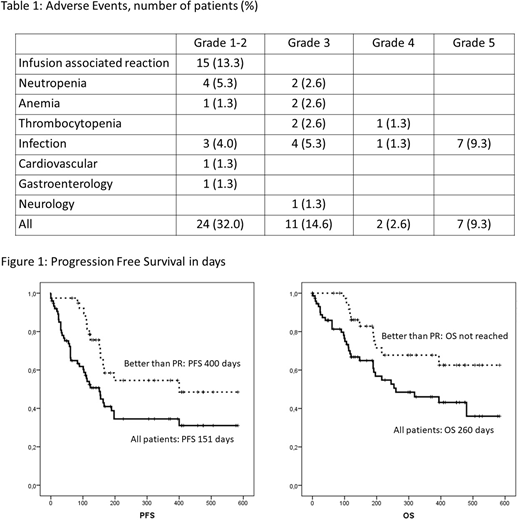
Results: 8 centers responded with 75 patients altogether. Patients were heavily pretreated, the median number of prior lines was 3 (1-12). All patients had prior bortezomib, and most had lenalidomide (82.6%) and thalidomide (86.6%), all but one had one of the two IMiDs. 62.6% of the patients had prior autologous transplantation, with two having prior allograft, as well. Pre-daratumumab cytogenetic FISH tests of 57 patients were available, here 33/57 had high risk cytogenetics. The majority had high international staging system (ISS) score: 8, 16 and 48 were in the ISS 1, 2 and 3 groups respectively. Treatment usually continued until progression, unacceptable toxicity or death, the mean number of cycles was 6. AEs over grade 3 were uncommon, the most frequent AEs were mild infusion associated reactions (IARs, grade 1-2) and infections (Table 1). There were 7 fatal infections, other fatal AEs were absent. Infusion related toxicities were manageable in all cases. The majority of patients (41) had monotherapy with dexamethasone only, but 17 had bortezomib and another 17 lenalidomide combination. Overall response rate was assessable in 66 patients with 7 complete, 8 very good partial, 24 partial, 5 minor responses. 14 showed stable disease, 8 progressive disease. 9 patients had no formal disease reassessment due to either early death or short follow up. There was no clear connection between the number of prior lines and the quality of the response, however those who had either bortezomib or lenalidomid combinations showed better overall response rate (p=0.045).
With 43 events so far the estimated PFS and OS were 151 and 260 days, but it was much better in those who showed at least a partial response (PFS 400 days, OS nor reached; Figure 1). The only other factor that significantly affected the PFS was ISS (p=0.039), we could not demonstrate a significant connection between cytogenetics, the number of prior lines, combination therapy and survival.
Conclusion: Our results highlight the differences between patients treated in routine practice and those treated in clinical trials. Here treatment protocols were dictated by funding rules, and therefore similar patients were treated with doublets and triplets. The results of the POLLUX and CASTOR trials were superior in comparison to the SIRIUS study with monotherapy, but our results do not reflect this marked difference, probably due to the almost complete absence of 2nd and 3rd line patients who dominated the Pollux and Castor trials. Importantly these heavily pretreated patients tolerated daratumumab well, IARs over grade 2 were absent. Based on our results, daratumumab is an effective treatment option for relapsed/refractory MM with good safety profile.
Masszi:Janssen-Cilag: Consultancy; Takeda: Consultancy; AbbVie: Consultancy; Pfizer: Consultancy; Novartis: Consultancy; BMS: Consultancy. Illés:Takeda: Membership on an entity's Board of Directors or advisory committees; Roche: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees; Janssen: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal